백일해, Pertussis (Whooping cough)
(You may visit www.drleepediatrics.com – Chapter 7,
Pediatric Adolescent Infectious Diseases or제 7권, 소아 청소년 감염병 질환 웹사이트)
백일해의 개요 및 원인

그림 2-73. 백일해를 앓는 아이가 말할 때나 기침할 때 비말 속에 든 백일해균이 다른 사람에게 전염될 수 있다. Copyright ⓒ 2011 John Sangwon Lee, MD., FAAP
-
백일해는 백일해균(보르데텔라 퍼르투시스 백일해균 Bordetella pertussis) 감염으로 생기는 상·하기도 감염병이다.
-
보르데텔라 퍼르투시스균 감염은 주로 비강·인두 등의 상기도와 기관·기관지 등 하기도의 점막층에 생긴다.
-
백일해균이 상·하 기도에 감염되면 급성 세균성 호흡기계 감염병이 생길 수 있다.
-
백일해를 앓고 있는 소아청소년들이나 성인들, 또는 그 세균을 보균한 사람이 기침을 할 때나 말을 할 때 그들 이 기침할 때 가래, 또는 비말(飛沫) 등에 섞여있는 백일해균을 기도 속으로 흡인할 때, 또는 감염된 환자가 가지고 놀던 장난감 등에 오염된 백일해균에 접촉되거나 그 백일해균이 흡인될 때 백일해균에 감염되어 백일해에 걸릴 수 있다.
-
백일해균 면역체가 없는 사람은 누구든 백일해균에 감염되어 백일해에 걸려 앓을 수 있다. 다시 말하면 성인들, 사춘기 아이들, 학령기 아이들, 영유아들 연령을 가릴 것 없이 백일해균 감염에 면역이 없으면 누구든지 백일해균에 감염되어 백일해를 앓을 수 있다.
-
생후 3개월에서 4세까지 영유아들은 백일해에 더 잘 걸릴 수 있다.
-
그렇지만 6세 이후 학령기 아이들이나 사춘기 아이들도 백일해에 걸릴 수 있다.
-
또 요즘은 백일해 백신으로 기본 예방접종을 받고 백일해에 예방되었던 사춘기 전후 아이들이나 성인들에게 백일해가 발생되기도 하고 그로 인해 비전형적 백일해(Atypical pertussis)의 증상 징후가 나타나기도 한다.
-
잠복기는 약 6∼21일이다. 평균 7~10일이다.
백일해의 증상 징후
-
백일해의 증상 징후는 환자의 나이에 따라 다르다.
-
치료의 여부, 치료의 효과, 기본 예방접종 배열을 완전히 받았는지, 병일 수, 합병증의 유무 등에 따라 다르다.
-
또 예방접종을 조금도 받지 않은 아이들에게 생기는 전형적 백일해, 백일해 예방접종 배열 스케줄에 따라 완전히 접종 받은 후 백일해균에 면역력이 약해지거나 면역력이 없어질 때 백일해균에 감염되어 생기는 비전형적 백일해 등이 있다.
-
이상 설명한 백일해의 종류들 중 어떤 종류의 백일해에 걸려 앓고 있느냐에 따라 증상 징후가 다르다.
-
또 사춘기 아이들이나 성인들에게 생기는 백일해의 증상 징후는 영유아들에게 생기는 백일해의 증상 징후와 다른 점이 많다.
사진 2-74. 백일해를 일으키는 백일해균 그람 염색 현미경 세균검사.출처–미 CDC
-
백일해의 전형적인 증상 징후는 다음과 같다.
-
콧물, 경도 기침, 미열 등의 증상을 동반하는 카타르기(Catarrhal stage)가 제일 먼저 생기고 이 카타르기는 1~2주 동안 지속되는 것이 보통이다.
-
그 다음 경해기(Paroxysmal stage)가 온다. 경해기 동안에는 발작성 기침 후 구토, 흡기성 협착음과 천명이 주로 생긴다.
-
기침하는 도중에 구토도 한다.
-
보통 열은 없거나 미열이 날 수 있다.
-
경해기는 보통 1~6주간 계속 된다.
- 그 다음에는 회복기(Convalescent stage)로 접어든다. 회복기는 3주 동안 가는 것이 보통이다.
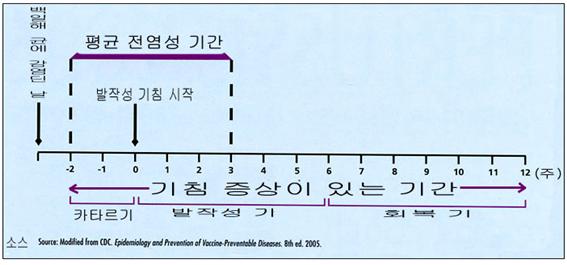
그림 2-75.백일해를 앓는 일수에 따른 전형적인 증상
-
회복기 동안에는 기침을 이전보다 덜 앓고 점점 기침을 덜 하면서 완전히 회복 될 수 있다.
-
증상을 다시 구체적으로 설명하면 이렇다.
-
초기 여러 날 동안은 감기를 앓을 때와 비슷하게 증상 징후와 콧물이 나고 기침을 조금씩 할 수 있다.
-
그 후 여러 날 동안 경련성 기침을 심하게 한다.
-
그 다음 여러 날 동안은 회복기로 접어든다.
-
이 병의 초기에는 열이 거의 나지 않거나 미열이 날 수 있고, 기침을 조금씩 하고 콧물이 난다.
-
병이 점점 더 진행되면서 백일해균 기관지염이 생기고 때로는 얼굴이 창백해진다.
-
경련성 기침을 심하게 할 때 결막하 모세혈관이 파열되어 결막하 출혈([부모도 반의사가 되어야 한다–소아가정간호백과]-제19권 소아청소년 안과 질환–결막하 출혈 참고)이 생길 수 있다.
-
이 시기에 경련성 기침이 2∼3분간 심하고 끈질기게 지속되다가 기절 할 수 있다.
-
때로는 기침을 심하게 하기 때문에 잠도 제대로 잘 수 없다.
-
식욕 부진으로 음식물을 잘 먹지 못해 기운이 없고 몸이 축 늘어지기도 한다.
-
합병증이 없는 한 이런 증상 징후들은 약 6∼10주간 계속되다가 자연히 회복될 수 있다.
-
생후 6개월 이전 영아들이 백일해에 걸리면 생명이 위험할 정도로 심하게 앓을 수 있다.
-
최근 백일해 백신으로 예방접종을 받지 않은 생후 0~6개월 된 신생아들이나 영아들이 백일해에 걸려 심하게 앓거나 심지어 사망까지 할 수 있다.
-
영아들이 백일해에 걸리면 심한 호흡곤란이 생기고 무호흡증도 생길 수 있다.
사진 2-76. 백일해로 심히 기침을 한다
출처-WHO and Infectious Diseases In Children, November, 2002
백일해의 합병증
-
백일해를 앓는 중 기절, 수면장애, 오줌 싸기, 늑골 골절, 뇌병증, 폐렴·중이염·전신경련·두개강 내 뇌출혈 등이나 그 외 다른 여러 종류의 합병증이 생길 수 있다.
-
갑자기 사망 할 수 있다.
백일해의 진단
-
병력·증상 징후·진찰소견 등을 종합해서 백일해가 의심되면 그람 염색 현미경 세균검사, 백일해균 세균배양 검사와 직접형 형광항체법 검사, DNA 검사, 면역글로불린 G 검사, PCR 검사 등으로 진단할 수 있다.
-
이 중 백일해균 세균배양 검사가 진단 상 가장 정확하고 신빙성이 있다.
-
백일해를 앓는 환아를 과거에 단 한 번쯤 목격한 사람은 백일해 환아가 기침하는 소리만 듣고서도 금방 백일해를 앓고 있다고 진단할 수 있을 정도로 백일해 기침은 특이하다.
-
심한 백일해 기침은 거의가 경련성 흡기성 기침이다.
-
적절한 혈액 임상검사를 하고 비강 맨 뒤 부위(비강인두 부위)의 점막층에서 다크론 알지네이트 면봉으로 점액을 조금 채취하거나 기침할 때 나온 가래와 비말로 백일해균 세균 배양검사를 특별히 해 백일해를 확진할 수 있다.
백일해의 치료
-
이 병을 앓고 있다고 의심되면 의사에게 곧 문의하여 진단 치료를 받아야 한다.
-
생후 6개월 이전 영아들이 백일해에 걸리면 폐렴(22%), 전신경련(2%), 뇌 병변(<2%) 생길 수 있고 무호흡증, 저산소증, 식이 문제 등이 생길 수 있고 그 외 다른 합병증이 생길 수 있으므로 병원에 입원해 적극적인 치료를 받아야 한다.
-
백일해의 발병 초기에 Erythromycin이나 Azithromycin, 또는 Clarithromycin 등의 항생제들 중 한 종류를 선택해 치료하는 것이 보통이다.
-
때로는 TMP-SMX로 치료한다.
-
생후 1개월 이전 신생아의 백일해를 치료하는 데 Erythromycin으로 치료할 수 있으나 유문 비대증 발병 등의 부작용이 그 항생제 치료로 생길 수 있다.
-
이런 치료로 환자의 신체 내 백일해균이 더 증식되지 못하게 해서 다른 사람들에게 덜 감염시킬 수 있고 백일해 증상 징후도 다소 호전될 수 있다.
-
그러나 항생제 치료로 백일해가 완치되지 않는 것이 보통이다.
-
백일해가 완치되기 전에 어느 종류의 항생제 치료로도 백일해의 자연 진행과정을 더 이상 진행되지 않게 막아 백일해를 속히 낫게 할 수 있는 백일해 특효치료약은 아직 없다.
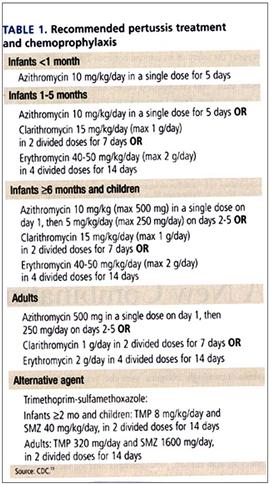
표 2-12. 백일해 항생제 치료와 예방적 화학요법(영문). 출처–미 CDC
-
발병 초기에 확실하게 진단을 하지 못해 에리스로마이신 등 항생제로 치료하지 못하고 그냥 지나칠 수 있다.
-
경련성 기침을 할 때까지 백일해가 많이 진행된 후에는 에리스로마이신으로 치료해도 별 치료효과가 없다.
-
백일해를 앓는 동안 잘 먹지 못할 수 있다.
-
영양분을 충분히 보충해 주기 위해서 맛있고 색다른 음식물을 나이에 따라 골고루 자주 주어야 한다.
-
탈수가 되지 않도록 음료수도 조금씩 자주 주어야 한다.
-
의사의 지시에 따라, 항염증제인 코르티코스테로이드제와 기관지 확장 작용제 알부테롤 등으로 치료해볼 수 있다. 그리고 다른 종류의 기침약으로 치료해볼 수 있다.
-
그러나 코데인이나 하이코민 등 강력한 기침약으로 치료하는 것은 권장하지 않는다.
백일해 환아의 격리
-
일단 발병된 후, 기침을 거의 하지 않을 때까지 약 6∼10주 정도 걸린다.
-
이병을 앓는 동안, 백일해 환자를 격리시키는 것이 좋다.
-
에리스로마이신 등 항생제 치료를 시작한 5∼10일이 지난 후 더 이상 격리시킬 필요가 없다.
백일해 환아와 접촉했거나 근접했을 경우
-
백일해 백신으로 백일해 예방접종 배열을 권장한 대로 접종 받지 않은 4∼7세의 아이가 백일해 환자와 접촉했을 때는 의사의 처방에 따라 에리스로마이신이나 아목시실린, 또는 다른 적절한 항생제로 이 병을 일시적으로 예방적 항생제 치료를 한다.
-
권장한 대로 적기에 백일해 예방접종 배열을 완전히 마치지 않은 아이들에게 나머지 백일해 예방접종 백신을 다 접종해야 한다.
백일해 예방 접종
-
2013년 미 소아청소년과 학회에서 권장하는 소아청소년 감염병 예방접종 참조
-
최근, 백일해를 앓는 아이들을 보기 힘들 정도다. 그러나 백일해 백신으로 예방접종을 한 번도 받지 않은 영유아들이나 학령기 아이들, 사춘기 아이들, 또는 성인들에게 백일해가 생길 수 있다. 또 권장한 대로 DTaP 백신을 권장 예방접종 배열에 따라 적기에 받았던 사춘기 아이들과 성인들에게도 백일해가 드물게 발생되고 있다. 또 백일해 예방접종을 권장한 대로 받지 않은 아이들이나 성인들이 백일해에 걸려 고생하기도 한다.
-
DTaP 백신은 생후 2·4·6 개월에 각각 1차, 2차, 3차로 총 3차 접종해 준다.
-
그 다음 생후 15~18개월에 4차 접종해 주고 4∼6세에 DTaP 백신으로 5차 접종을 받으면 백일해뿐 아니라 파상풍과 디프테리아도 예방될 수 있다.
-
요즘 백일해에 걸리는 아이들의 대부분은 여러 가지의 이유로 백일해 백신으로 예방접종 배열을 적기에 권장한대로 완전히 다 받지 못해서 백일해에 걸리는 경우가 대부분이다. 백일해 백신으로 예방접종을 해 준 후 심한 부작용이 생겨 백일해 백신예방접종을 더 이상 접종해 줄 수 없는 경우도 가끔 있다. 다음 Adacel 백신이나 Boostrix 백신의 예방 접종을 참조.
| Update 업데이트
Pediarix는 디프테리아, 파상풍, 백일해, B형 간염, 소아마비에 대한 예방 접종을 할 수 있는 종합 백신이다. Pediarix는 B형 간염 표면 항원 음성인 산모로부터 태어난 영아 6주부터 6세까지 3회 접종할 수 있다. Pediarix is a combined vaccine that provides vaccination against diphtheria, tetanus, pertussis, hepatitis B, and polio. Pediarix can be administered in three doses from 6 weeks to 6 years of age for infants born to mothers who are hepatitis B surface antigen-negative. |
Pertussis (Whooping cough) 백일해
Overview and causes of whooping cough

Figure 2-73. When a child with whooping cough speaks or coughs, the pertussis bacteria in the droplets can be transmitted to others. Copyright ⓒ 2011 John Sangwon Lee, MD., FAAP
• Pertussis is an upper and lower respiratory tract infection caused by pertussis (Bordetella pertussis) infection.
• Bordetella pertussis infection mainly occurs in the mucous membranes of the upper respiratory tract such as the nasal cavity and pharynx and the lower respiratory tract such as the trachea and bronchi.
• Pertussis infection in the upper and lower airways can lead to acute bacterial respiratory infections.
• When children and adolescents or adults with whooping cough, or a person carrying the germ, cough or talk when they cough, aspirate whooping cough bacteria mixed with sputum or droplets into the airways. When the infected patient comes into contact with contaminated pertussis or is aspirated by pertussis, it is possible to become infected with pertussis and get pertussis.
• Anyone who does not have the pertussis immune system can become infected with pertussis and suffer from whooping cough. In other words, adults, adolescents, school-age children, and infants regardless of age, who are not immune to whooping cough infection, can become infected with whooping cough and suffer from whooping cough.
• Infants and toddlers aged 3 months to 4 years of age are more susceptible to whooping cough.
• However, school-age children and adolescent children after the age of 6 can also get whooping cough.
• Nowadays, pertussis may occur in children and adults before and after puberty who received basic vaccination with whooping cough vaccine and were prevented from whooping cough, resulting in symptoms of atypical pertussis.
• The incubation period is about 6 to 21 days. It averages 7-10 days.
Symptoms, signs of whooping cough
• Symptoms of whooping cough depend on the age of the patient.
• Depends on treatment, the effectiveness of treatment, complete basic immunization arrangement, number of illnesses, and complications.
• In addition, there are typical whooping cough, which occurs in children who have not yet been vaccinated, and atypical whooping cough, which occurs when immunity to whooping cough is weakened or immunity is lost after receiving a complete vaccination according to the whooping cough vaccination schedule.
• Symptoms of whooping cough are different depending on the type of whooping cough described above.
• In addition, the symptoms of whooping cough in adolescent children and adults are different from those of whooping cough in infants and young children.
Photo 2-74. Pertussis bacteria causing whooping cough. Gram stain microscopic bacterial examination. Source-US CDC
Typical symptoms of whooping cough include the following.
• Catarrhal stage, which is accompanied by symptoms such as runny nose, mild cough, and mild fever, occurs first and usually lasts for 1 to 2 weeks.
• Then comes the Paroxysmal stage.
Vomiting, inspiratory strictures and wheezing occur mainly after paroxysmal coughing during the period of invigoration.
• Vomiting while coughing.
• Usually no fever or mild fever.
• The light sea period usually lasts for 1 to 6 weeks.
• After that, it enters the convalescent stage. The recovery period usually lasts for 3 weeks.
2-75.백일해를 앓는 일수에 따른 전형적인 증상
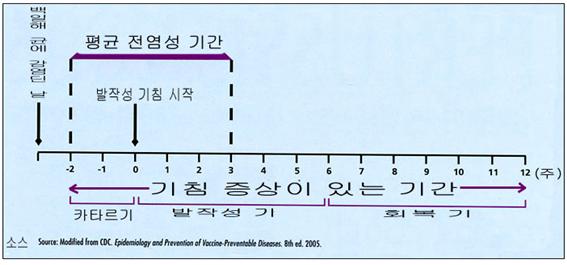
Figure 2-75. Typical symptoms depending on the number of days pertussis
• During the recovery period, you can recover completely with less coughing than before and gradually less coughing.
• Here is the detailed description of the symptoms.
• During the first few days, you may have symptoms and a runny nose and cough little by little, similar to when you have a cold.
• You have a convulsive cough for several days thereafter.
• The next few days go into a recovery phase.
• At the beginning of the disease, you may have little or no fever, cough little by little, and runny nose.
• As the disease progresses, pertussis bronchitis develops and sometimes the face becomes pale.
• When convulsive coughing is severe, subconjunctival capillaries may rupture, resulting in subconjunctival bleeding ([Parents should also become at least the half-doctors-Pediatrics and Family Nursing Encyclopedia)-Vol. 19 Child and Adolescent Eye Diseases-Subconjunctival bleeding).
• During this time, a convulsive cough may last for 2 to 3 minutes and then pass out.
• Sometimes I cough severely, so He can’t sleep well.
• Due to poor appetite, he can’t eat well, so he doesn’t have energy and his body is drooping.
• Unless there are complications, these symptoms may continue for about 6 to 10 weeks before recovering spontaneously.
• Infants before 6 months of age can get sick with whooping cough, which is life-threatening.
• Newborns and infants aged 0-6 months who have not been vaccinated with the recent whooping cough vaccine can get seriously ill or even die from whooping cough.
• When infants develop whooping cough, they may develop severe breathing difficulties and may develop apnea.
Photo 2-76. Coughing severely from whooping cough. Source-WHO and Infectious Diseases In Children, November 2002
Complications of whooping cough
• Whooping cough can cause fainting, sleep disturbances, peeing, rib fractures, encephalopathy, pneumonia, otitis media, general nervous system cramps, cerebral hemorrhage in the cranial cavity, and many other complications.
• Sudden death can occur.
Diagnosis of whooping cough
• If whooping cough is suspected by combining medical history, symptoms, and examination findings, it can be diagnosed by Gram staining microscopy bacterial test, pertussis bacterial culture test, direct fluorescent antibody test, DNA test, immunoglobulin G test, PCR test, etc. have.
• Among them, the pertussis bacteria culture test is the most accurate and reliable in diagnosis.
• Whooping cough is so unusual that a person who has seen a child suffering from whooping cough at least once in the past can be diagnosed as having whooping cough soon after hearing the sound of the child with whooping cough.
• Severe whooping cough is almost always a convulsive inspiratory cough.
• Pertussis can be confirmed by performing appropriate blood clinical tests and collecting a small amount of mucus from the mucous layer at the back of the nasal cavity (in the nasopharynx) with a dacron alginate swab or performing a pertussis bacterial culture test using sputum and droplets from coughing. have.
Treatment of whooping cough
• If you suspect you have this disease, you should contact your child’s doctor right away for diagnostic treatment.
• If infants before 6 months of age have whooping cough, pneumonia (22%), systemic cramps (2%), brain lesions (<2%), apnea, hypoxia, dietary problems, and other complications may occur. Because of this, you must be admitted to the hospital and receive active treatment.
• In the early onset of whooping cough, it is common to choose one of the antibiotics such as Erythromycin, Azithromycin, or Clarithromycin to be treated.
• Sometimes treated with TMP-SMX.
• Erythromycin can be used to treat whooping cough in newborns before 1 month of age, but side effects such as the onset of pyloric enlargement can occur with antibiotic treatment.
• These treatments can prevent more proliferation of pertussis bacteria in the patient’s body, making them less infectious to others, and may improve the symptoms of whooping cough somewhat.
• However, antibiotic treatment does not usually cure whooping cough.
• Before pertussis is cured, there are no special treatments for whooping cough that can quickly cure whooping cough by stopping the natural process of whooping cough with any type of antibiotic treatment.
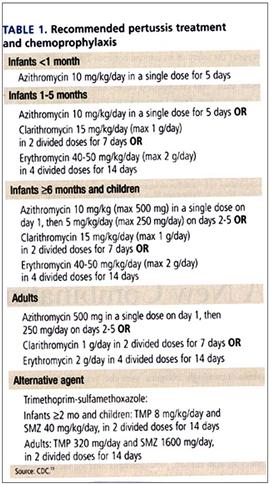
Table 2-12. Pertussis Antibiotic Treatment and Prophylactic Chemotherapy (English). Source-US CDC
• Since the diagnosis cannot be made clear at the beginning of the onset, treatment with antibiotics such as erythromycin may not be possible and may be overlooked.
• After whooping cough has progressed a lot until convulsive coughing, treatment with erythromycin does not have any therapeutic effect.
• You may not be able to eat well while suffering from whooping cough.
• In order to sufficiently replenish nutrients, delicious and unusual foods should be given often and evenly according to age.
• Drinking water should be given little by little and often to prevent dehydration.
• As directed by your doctor, treatment with anti-inflammatory drugs such as corticosteroids and bronchodilating agents albuterol. And you can treat it with other types of cough medicine.
• However, treatment with strong cough medicines such as codeine or hycomine is not recommended.
Isolation of children with whooping cough
• Once onset, it takes about 6 to 10 weeks until you rarely cough.
• While suffering from this disease, it is advisable to isolate the person with whooping cough.
• It is no longer necessary to quarantine 5 to 10 days after starting treatment with antibiotics such as erythromycin.
In case of contact with or close to a child with whooping cough
• If a 4-7-year-old child who has not been vaccinated as recommended for whooping cough vaccination arrangements with whooping cough vaccine comes into contact with a whooping cough patient, temporarily prevent the disease with erythromycin, amoxicillin, or other appropriate antibiotics as prescribed by a doctor. Take antibiotic treatment.
• Children who have not completed the pertussis vaccination arrangement in a timely manner as recommended should be vaccinated against the remaining whooping cough vaccinations. Whooping cough vaccination
• Refer to the pediatric and adolescent infectious disease
Vaccination recommended
by the American Academy of Pediatrics and Adolescents in 2013.
• Recently, it is hard to see children suffering from whooping cough. However, whooping cough can develop in infants, school-age children, adolescents, or adults who have never been vaccinated with the whooping cough vaccine. In addition, whooping cough is rare in adolescent children and adults who received DTaP vaccine in a timely manner according to the recommended vaccination arrangement as recommended.
Also, children and adults who have not received the whooping cough vaccination as recommended are suffering from whooping cough.
• DTaP vaccine is given at 2, 4 and 6 months of age, with a total of 3 doses, 1st, 2nd, and 3rd doses respectively.
• Then, 4th vaccination at 15-18 months of age and 5th vaccination with DTaP vaccine at 4-6 years of age can prevent not only whooping cough, but also tetanus and diphtheria.
• Most of the children who get whooping cough these days do not get all of the immunization arrangements with the whooping cough vaccine in a timely manner as recommended for a number of reasons, so they develop whooping cough.
In some cases, after vaccination with the whooping cough vaccine, severe side effects occur, and the whooping cough vaccination can no longer be vaccinated. See vaccination with the following Adacel vaccine or Boostrix vaccine.
Recommended immunization schedule for persons aged 0 through 18 years since January 2021,
2021년 1월 이후 권장 미 0~18세 소아청소년 기본 예방접종 스케줄과 표 1A
Vaccination type of vaccine/ infectious disease that prevent
| Vaccination type of vaccine/ infectious disease that prevent | Right after birth | After birth 1 month | After birth 4 month | After birth 6 month | After birth 9 month | After birth 12 month | After birth 1 5 month | After birth 18 month | After birth 19~23 month | After birth 2-3 years old | After birth 4-6 years old | After birth 7-10 years old | After birth 11-12 years old | After birth 13-15 years old | After birth 16-18 years old | |||||||
| Hepatitis B¹ (HepB) /b 형 간염 | ←1st vaccination→ | ←2nd vaccination→ | ←←3rd vaccination→→ | |||||||||||||||||||
| Rotavirus² (RV) RV-1 (two batch sequence inoculation); RV-5 (3-batch sequence vaccination)/ Rotavirus infection | ←1st vaccination→ | ←2nd vaccination→ | note 2 | |||||||||||||||||||
| Diphtheria, Tetanus, acellular Pertussis³ (DTaP; <7 years old)/tetanus, diphtheria, pertussi | ←1st vaccination→ | ←2nd vaccination→ | ←3rd vaccination→ | ←4th vaccination→ | ←5th vaccination→ | |||||||||||||||||
| Tetanus, Diphtheria, acellular Pertussis⁴ (DTap; 7 years old> 7 years old tetanus, diphtheria, whooping cough | (Tdap) | |||||||||||||||||||||
| Haemophilus influenzae type b⁵(HIb)/ Hib infectious disease | ←1st vaccination→ | ←2nd vaccination→ | note 5 | ←3rd or 4th vaccination→ Footnote 5 | ||||||||||||||||||
| Pneumococcal conjugate⁶a, c (PCV13)/Pneumococcal infection | ←1st vaccination→ | ←2nd vaccination→ | ←3rd vaccination→ | ←4th vaccination→ | ||||||||||||||||||
| Pneumococcal polysaccharide⁶bc (PPSV23) / Streptococcal pneumonia infection | ||||||||||||||||||||||
| Inactivated Poliovirus⁷(IPV)(<18 years old)/Polio | ←1st vaccination→ | ←2nd vaccination→ | ←3rd vaccination→ | ←4th vaccination→ | ||||||||||||||||||
| Vaccination type of vaccine/ infectious disease that prevent | Right after birth | After birth 1 month | After birth 2 month | After birth 4 month | After birth 6 month | After birth 9 month | After birth 12 month | After birth 15 month | After birth 18 month | After birth 19-23 month | After birth 2-3 years old | After birth 4-6 years old | After birth 7-10 years old | After birth 11-12 years old | After birth 13-15 years old | After birth 16-18 years old | ||
| Influenza⁸ (IIV; LAIV) for 1 copy, 2 servings, footnote 8 / Influenza | ←Get inoculated every year (11V 만)→ | ←Get inoculated every year(II V or LAIV)→ | ||||||||||||||||
| Measles, Mumps, Rubella⁹(MMR)/ Measles, Rubella, Mumps | ←1st vaccination→ | ←2nd vaccination→ | ||||||||||||||||
| Varicella ¹⁰ (VAR) /Varicella | ←1st vaccination→ | ←2nd vaccination→ | ||||||||||||||||
| Hepatitis A¹¹ (HepA)/Hepatitis A | ←2 doses→ | |||||||||||||||||
| (Human papillomavirus¹² (HPV2; women only (HPV4; women and men))/Human papillomavirus infectious disease | ←3rd vaccination→ | |||||||||||||||||
| Meningococcal¹³ (MenACWY-D 9 months or later. MenACWY-CRM-D is 2 months or later. MenACWY-TT is 2 years old or later. / Meningococcal meningitis and other infectious diseases) —————————- Meningococcal B vaccines include MenB-4C, Bexsero, MenB-FHbp, and Trumenba vaccines. We touch on 10 years of age or older. The Bexsero vaccine is inoculated twice and the Trumenba vaccine has inoculated a total of three times. Adolescents and young adults with no risk are vaccinated at age 16-23. Source: CDC, AAP News 3/2021 | ←1st vaccination→ | Booster vaccination | ||||||||||||||||
|
|
The age range for which vaccination is recommended, | ||
|
|
Age recommending vaccination for children in the high-risk group |
DTaP vaccine (diphtheria, whooping cough, tetanus vaccine) vaccination
Diphtheria, Tetanus, Acellular Pertussis Immunization
• The DTaP vaccination vaccine is a comprehensive vaccination vaccine that can prevent diphtheria, whooping cough, and tetanus. DTaP is an abbreviation of D for Diphtheria, T for Tetanus, A for Acellular, and P for Pertussis.
• An oral DTaP vaccination vaccine has not yet been developed. Vaccination age

Photo 2-77. DTaP vaccination vaccine and syringe Copyright ⓒ 2011 John Sangwon Lee, MD, FAAP
• DTaP vaccination is given at 2, 4, 6, 15~18 months and 4~6 years of age, with a total of 5 doses, 1st, 2nd, 3rd, 4th and 5th doses, respectively.
• Every 10 years from the date of last DTaP vaccination, get the Td vaccine to prevent tetanus and diphtheria, or the Tdap vaccine to prevent diphtheria, whooping cough, and tetanus.
• As new pertussis vaccination vaccines are frequently developed and vaccination methods are changed, vaccinations with pertussis vaccines should be given according to the instructions of a regular doctor.
Latest information on how to get vaccinated against whooping cough vaccine
• Two new DTaP vaccines that can be vaccinated with diphtheria, tetanus and whooping cough vaccines to adolescent children and adults have been approved by the US FDA.
• One is the Boostrix vaccine made by GlaxoSmithKline Pharmaceuticals, and the other is the Adacel vaccine made by Sanofi Pasteur Pharmaceuticals.
The Boostrix DTaP vaccine can be given the first dose to adolescent children and adults aged 10-18 years, and the Adacel DTaP vaccine is available for the first dose to children and adults aged 11 to 64 years.
Previously, it was recommended to prevent diphtheria and tetanus with Td vaccine 10 years after receiving the last DTaP vaccine at 5-6 years of age, and pertussis vaccination is no longer recommended after 5-6 years of age. Did.
• As recommended in the past, children who were vaccinated against diphtheria, tetanus, and whooping cough vaccinations prior to puberty before puberty may develop whooping cough after puberty and adults may develop whooping cough.
Therefore, recently, it is recommended that adolescent children and adults be vaccinated once with the Adacel vaccine or Boostrix vaccine, which is a comprehensive DTaP vaccination vaccine.
• When vaccinating children or adults aged 10-18 years old with the Td vaccination vaccine, they can be vaccinated with the DTaP vaccine, Adacel vaccine or Boostrix vaccine, instead of the Td vaccination vaccine.
• Therefore, when children aged 10 to 18 need to be vaccinated against TD, they should consult with their doctor to immunize them with Adacel vaccine or Boostrix vaccine.
How to get vaccinated against whooping cough vaccine
• Get a health checkup and take your temperature to see if you have a fever.
• If there is no fever and there are no contraindications to receiving DTaP vaccine, 0.5cc of DTaP vaccine should be inoculated by intramuscular injection of the thigh or upper arm.
• If you have an acute febrile infection, it is not recommended to get the DTaP vaccine. After that, take it after the disease is healed.
• You can get the DTaP vaccine as directed by your doctor even if you have a mild cold or other types of viral respiratory diseases other than a cold.
• If you have had a high fever of 40 degrees Celsius or higher from DTaP vaccine after receiving DTaP vaccine in the past, or if you have a history of serious other side effects, you will not be able to get the next DTaP vaccine.
• If you have had side effects of any kind after receiving DTaP vaccine in the past, you should tell your doctor about the side effects of DTaP in detail.
A compound vaccine to prevent bacterial and viral infectious diseases
• Pediarix (Diphtheria, Tetanus Toxoids, Acellular Pertussis Adsorbed, Hepatitis B (Recombinant), Inactivated Poliovirus Vaccine Combined) vaccine is a type of comprehensive vaccine that can be vaccinated against diphtheria, tetanus, pertussis, hepatitis B, and polio.
• Previously, to prevent diphtheria, whooping cough, polio, and hepatitis B, the first vaccination was given separately with 3 injections. Instead of receiving 3 injections in the past, the Pediarix comprehensive vaccine was used to immunize 5 types of infectious diseases with one injection. can do.
• At 2, 4, and 6 months of age, the Pediarix comprehensive vaccine can be given at the first, second and third doses, respectively.
• Children 7 years of age or older cannot be vaccinated with the Pediarix comprehensive vaccine.
• Since new vaccines are frequently developed, pediatricians and adolescents vaccinate children and adolescents, and they refer to the latest vaccination reference books whenever they are vaccinated. These days, the current situation is that vaccinations are given to children and adolescents.
The last whooping cough vaccination is usually given around the age of 4-6. After 5 to 10 years, the pertussis immunity may gradually decrease. So, adolescent children and adults can get whooping cough. The American Academy of Pediatrics and Adolescents recommends that children and adolescents who have received the DTP/DTaP vaccine as recommended for the basic vaccination arrangement before puberty are simultaneously prevented with the DTap vaccine at the age of 11-18. It is usually recommended to inoculate at the age of 11-12.
Vaccination side effects
• Depending on the type of vaccination vaccine, side effects may appear differently.
• The injection site may be sore, red, and swollen. You can get a fever and get sick.
Contraindications to vaccination
• Among the components of the DTaP vaccine, it may contain components such as yeast (fungus), Neomycin, and Polymyxin B. Children who are allergic to such ingredients should not be vaccinated with this vaccine. Vaccination contraindications vary depending on the type of vaccine.
• For more information, please refer to the January 2011 CDC and Child and Adolescent Vaccination Schedule Table (1). (2), (3). See (4). And see www.aapnews.org.
Minor side effects
• After receiving the DTaP vaccine, serious side effects due to the vaccination are not common, but the following minor side effects can be relatively common.
• The area that was injected with the DTaP vaccine may be slightly swollen and painful. The vaccinated leg may hurt enough to be unable to move properly for 1 to 3 days, and it may be suffocated with a mild fever.
Severe side effects
• If the following side effects occur after receiving the DTaP vaccine, it is called a serious and severe DTaP vaccine side effect.
• Have a high fever of 40 degrees Celsius (104 degrees Fahrenheit) or higher
• After receiving the DTaP vaccination, crying severely for more than 3 hours without being able to heal in any way • whether you are in shock
• having general cramps
• encephalitis
• anaphylaxis develops or
• Platelets or red blood cells are destroyed or
• etc
How to treat severe DTaP vaccine side effects
• To prevent tetanus, diphtheria, and whooping cough after receiving the DTaP vaccine, children who have had side effects from the severe DTaP vaccine can no longer be vaccinated with the DTaP vaccine.
However, among the components of the comprehensive DTaP vaccine, a TD vaccine that does not contain P, a pertussis vaccine, can be vaccinated against tetanus and diphtheria.
Record the serious side effects of getting vaccinated with the DTaP vaccine in detail on the immunization record card.
Then, before getting the DTaP vaccine, you should tell your doctor that you have had severe DTaP vaccine side effects. Children younger than 7 years old who received DTaP vaccine in the past and had severe DTaP vaccine side effects are vaccinated with a TD vaccine that does not contain the P component of whooping cough vaccine to vaccinate against tetanus and diphtheria. When the child is vaccinated with the TD vaccine due to severe DTaP vaccine side effects, the child is not immune to whooping cough because the child does not have an immune system that can prevent whooping cough.
Td vaccine and TD vaccine
- There are two types of TDI vaccines used to prevent tetanus and diphtheria. One is the Td vaccine and the other is the TD vaccine.
• TD vaccine or Td vaccine does not contain the P vaccine component, which can prevent whooping cough, but contains the tetanus vaccine, T vaccine component, and the diphtheria vaccine component D.
• In other words, T is for the tetanus vaccine and D is for the diphtheria vaccine.
• The main components of both Td and TD vaccines are tetanus (T) vaccine and diphtheria (D) vaccine.
• The amount of D vaccine contained in the Td vaccine is slightly higher than that of the active ingredient in the TD vaccine.
• Children under the age of 7 who are no longer vaccinated against diphtheria, tetanus, and whooping cough due to a side effect of the P (pertussis) vaccine contained in the DTaP vaccine can be vaccinated with the TD vaccine. Children and adolescents with abnormalities and adults can be vaccinated with the Td vaccine.
• Sometimes you can get vaccinated with tetanus vaccine T if you don’t prevent diphtheria, but only tetanus.
• Tetanus can occur when bacteria that cause tetanus enter the body through wounds such as abrasions, cuts, burns, and cuts.
• If you have suffered this type of trauma, you should be vaccinated with tetanus vaccine as recommended to see if you are completely immune to tetanus.
• If you are not immunized to tetanus because you have not been immunized with tetanus vaccine, TDI vaccine, or DTaP vaccine as recommended, you may get tetanus.
• In Pakistan these days, many children who were traumatized by earthquakes have suffered a lot of tetanus, and many died, the WHO reported.
- Vexelis Vaccine can be given( update 2022)
출처 및 참조 문헌 Sources and references
- NelsonTextbook of Pediatrics 22ND Ed
- The Harriet Lane Handbook 22ND Ed
- Growth and development of the children
- Red Book 32nd Ed 2021-2024
- Neonatal Resuscitation, American Academy Pediatrics
-
www.drleepediatrics.com제7권. 소아청소년 감염병
-
Red book 29th-31st edition 2021
-
Nelson Text Book of Pediatrics 19th- 21st Edition
-
The Johns Hopkins Hospital, The Harriet Lane Handbook, 22nd edition
-
Childhood Emergencies in the Office, Hospital and Community, American Academy of Pediatrics
-
Emergency Medical Service for Children, By Ross Lab. May 1989. p.10
-
Emergency care, Harvey grant, and Robert Murray
-
Emergency Care Transportation of Sick and Injured American Academy of Orthopaedic Surgeons
-
Emergency Pediatrics A Guide to Ambulatory Care, Roger M. Barkin, Peter Rosen
-
Immediate care of the acutely ill and injured, Hugh E. Stephenson, Jr
-
The Critically Ill Child, Diagnosis and Management, Edited by Clement A. Smith
-
Emergency Medical Services for Children: The Role of the Primary Care Provider, America Academy of Pediatrics
-
Quick Reference To Pediatric Emergencies, Delmer J. Pascoe, M.D., Moses Grossman, M.D. with 26 contributors
-
Manual of Emergency Care
-
응급환자관리 정담미디어
-
소아가정간호백과–부모도 반의사가 되어야 한다, 이상원
-
Neonatal Resuscitation American heart Association
-
Neonatology Jeffrey J.Pomerance, C. Joan Richardson
-
Pediatric Resuscitation Pediatric Clinics of North America, Stephen M. Schexnayder, M.D.
-
Pediatric Critical Care, Pediatric Clinics of North America, James P. Orlowski, M.D.
-
Preparation for Birth. Beverly Savage and Dianna Smith
- Infectious disease of children, Saul Krugman, Samuel L Katz, Ann A. Gershon, Catherine Wilfert
-
The Harriet Lane Handbook 19th Edition
-
소아과학 대한교과서
-
제1권 소아청소년 응급의료 참조문헌과 출처
-
Other
Copyright ⓒ 2015 John Sangwon Lee, MD., FAAP
“부모도 반의사가 되어야 한다”-내용은 여러분들의 의사로부터 얻은 정보와 진료를 대신할 수 없습니다.
“The information contained in this publication should not be used as a substitute for the medical care and advice of your doctor. There may be variations in treatment that your doctor may recommend based on individual facts and circumstances. “Parental education is the best medicine.”